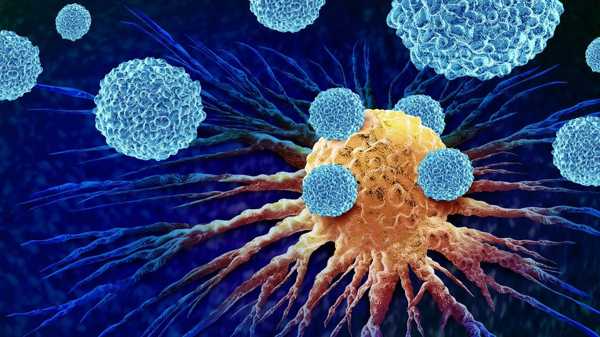
Cancer antibodies are transforming modern medicine, offering new possibilities for precise cancer diagnosis and therapy. These specially designed proteins can recognize and attach to cancer cells, marking them for destruction by the immune system. By enhancing the body’s natural defense mechanisms, antibody-based treatments provide a more targeted approach to cancer therapy—improving effectiveness, minimizing damage to healthy cells, and paving the way toward highly personalized cancer care.
Understanding Cancer Antibodies
Types of Cancer Antibodies
Cancer antibodies are categorized into several types, each serving a distinct therapeutic function:
• Monoclonal antibodies – These lab-generated antibodies are designed to target a single antigen. Their structural uniformity enables high specificity in recognizing cancer cells. They can directly block cancer growth or carry therapeutic agents such as toxins or radioactive materials to the tumor site for localized destruction.
• Bispecific antibodies – These antibodies can bind to two different antigens simultaneously. One end typically connects to a cancer cell, while the other binds to immune cells like T cells, enhancing the body’s immune response against tumors. This dual-targeting mechanism amplifies the immune attack and strengthens treatment efficacy.
• Conjugated antibodies – These antibodies are chemically linked to cytotoxic drugs or radioactive substances. Upon binding to cancer cells, they deliver their attached therapeutic agents directly into the malignant cells, providing localized treatment that spares surrounding healthy tissues.
Mechanisms of Action
Cancer antibodies eliminate malignant cells through several distinct biological mechanisms:
• Direct targeting – By attaching to specific molecules on the cancer cell surface, antibodies can interrupt key signals required for cell survival and proliferation, eventually leading to tumor cell death.
• Immune activation – Once antibodies bind to tumor cells, they attract immune components such as macrophages, T cells, or natural killer cells. This immune recognition prompts the destruction of cancer cells through a process known as antibody-dependent cellular cytotoxicity.
• Targeted drug delivery – In antibody-drug conjugates, antibodies function as transporters that guide toxic substances straight to cancerous cells. This strategy ensures that high concentrations of the therapeutic agent reach the tumor, maximizing impact while minimizing harm to non-cancerous tissues.
• Pathway disruption – Certain antibodies work by blocking signaling routes inside cancer cells that are responsible for growth and survival, effectively hindering tumor progression.
Applications in Immunotherapy
The use of antibodies in immunotherapy has reshaped cancer treatment by offering greater precision and reduced toxicity compared with traditional approaches. Notable examples include:
• Checkpoint inhibitors – These antibodies block inhibitory proteins like PD-1, PD-L1, and CTLA-4 that suppress immune responses. By removing these barriers, immune cells regain the ability to detect and destroy cancer cells effectively.
• Targeted therapeutic delivery – Conjugated antibodies are capable of transporting therapeutic agents directly to tumors, proving especially valuable for cancers that are resistant to systemic therapies.
• Combination therapies – Antibody-based treatments are frequently combined with other therapeutic methods, including chemotherapy, radiation, or additional immunotherapies. Such combinations often produce synergistic effects, leading to stronger tumor regression and improved long-term outcomes.
Advantages and Challenges
Cancer antibodies provide major therapeutic benefits. Their high specificity allows for precise targeting, reducing harm to healthy tissues. They can also be customized according to the molecular profile of a patient’s tumor, creating opportunities for more effective personalized treatments. Many cancers previously considered untreatable have shown improved response rates through antibody-based therapy.
However, challenges persist. Tumor cells may develop resistance by altering or reducing antigen expression, which limits treatment effectiveness. Producing therapeutic antibodies is also complex and expensive, as the process demands stringent quality control. Additionally, while generally safer than conventional treatments, antibodies can occasionally provoke immune-related side effects or inflammatory responses. Continued research is needed to enhance their safety and effectiveness, focusing on dosage optimization, improved targeting, and combined therapeutic strategies.
Research and Clinical Trials
Current research continues to expand the role of antibodies across various cancer types, including both solid and blood-related malignancies. Ongoing clinical trials explore new antigen targets, molecular modifications, and improved antibody designs to overcome treatment resistance. For instance, scientists are refining the Fc region of antibodies to enhance immune cell engagement and extend their activity in circulation.
There is also growing interest in understanding how antibodies interact with the tumor microenvironment—a complex system of immune cells, signaling molecules, and structural components surrounding cancer cells. Insights into this relationship are enabling the design of therapies that not only attack cancer cells directly but also reshape the tumor environment to favor immune activity. Collaboration among academic institutions, biotech companies, and healthcare organizations remains key to translating scientific breakthroughs into effective clinical solutions.
Future Directions
The future of antibody-based cancer therapy lies in greater precision, multifunctionality, and integration with other technologies. Researchers are developing next-generation antibodies capable of performing multiple tasks—such as modulating immune activity, altering the tumor microenvironment, and targeting several antigens simultaneously. Advances in genetic engineering and nanotechnology are expected to further improve antibody stability and delivery efficiency.
Personalized medicine will continue to shape the evolution of antibody therapies. By incorporating genetic data, biomarkers, and imaging technologies, clinicians will be able to tailor treatments to each patient’s unique tumor profile. This approach promises enhanced efficacy and fewer side effects.
New innovations, including bispecific antibodies and antibody cocktails, are also on the rise. These multi-targeted strategies reduce the chance of tumor escape and offer a more durable therapeutic response. As clinical evidence accumulates, antibody-based therapies will likely play an even more critical role in improving survival outcomes for patients across various cancer types.
Conclusion
Cancer antibodies have emerged as one of the most powerful advancements in oncology, offering the ability to specifically recognize and eliminate cancer cells while sparing healthy tissues. Despite challenges related to resistance and production, continued innovation in antibody engineering and clinical application is accelerating progress toward safer and more effective cancer therapies. As these treatments evolve and integrate with personalized approaches, cancer antibodies will remain at the forefront of modern oncology—reshaping the fight against cancer and enhancing the prospects for patients worldwide.